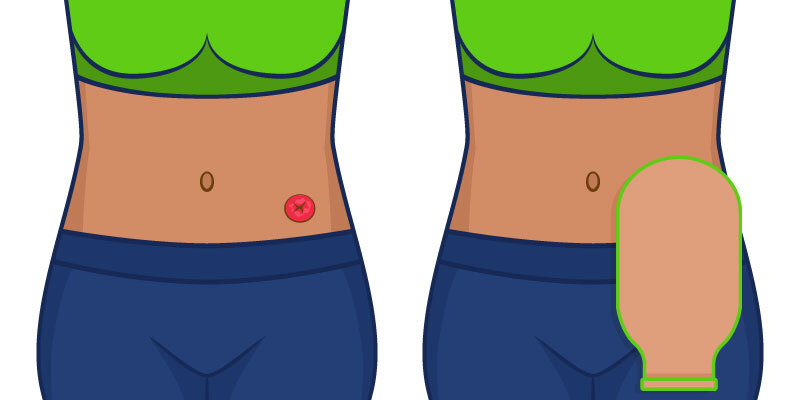
| Common Stoma Care Problems and Solutions16 January 2024 Once you get the hang of it, proper stoma care can be fairly easy. For the first few months following ostomy surgery, however, stoma care can be a daunting prospect. Learning how to recognise and deal with issues with your stoma can empower you to feel more confident in your ability to manage a stoma in the long-term. To get an understanding of some of the Common Stoma Care Problems and Solutions, we've put together this handy guide! What Will This Guide Cover
Parastomal HerniasA parastomal hernia is a hernia that forms around the stoma, and is fairly common following ostomy procedures. Some studies suggest that up to 78% of people develop a parastomal hernia within 2 years of surgery. Parastomal Hernia Symptoms Symptoms of a parastomal hernia include:
Cause(s) of Parastomal HerniasParastomal hernias form due to weakness in the abdominal wall and muscles. The hernia occurs when part of the bowel pushes through the muscle, and creates a swelling under the skin. There are various factors that can increase your risk of developing a parastomal hernia, including smoking, being overweight, heavy lifting, chronic coughing, long-term constipation, and developing a stoma infection. Parastomal Hernia Treatment and PreventionThe simplest treatment for parastomal hernias is to implement simple lifestyle changes such as quitting smoking, making a change to your diet or water-intake, or losing weight. Other treatment options involve seeking medical assistance to close, repair, or relocate the stoma, or to have a mesh insert surgically placed into or over the stoma. To prevent the development of a parastomal hernia, try using a stoma support belt to offer gentle compression and discreet, consistent support to the abdominal area. A stoma support belt can also help to manage and ease uncomfortable hernia symptoms during recovery. Recommended Stoma Support Belt for Parastomal Hernia Management: Deep Abdominal Binder Key Features of the Deep Abdominal Binder ✔ Adjustable design available in a range of sizes to ensure a secure fit Stoma InfectionsStoma infections, including bacterial, fungal, and viral infections, occur when the stoma area becomes contaminated by harmful micro-organisms. Stoma Infection Signs and SymptomsSymptoms and signs of stoma infections that it's important to look out for include:
Cause(s) of Stoma InfectionThe most common cause of stoma infections is inadequate hygiene in the area, but this doesn't necessarily mean that you'll only develop an infection if you don't clean your stoma. Things like stoma leakage and faecal contact with the skin can cause harmful micro-organisms to enter through broken skin. Stoma Infection Treatment and PreventionThe best way to prevent stoma infection is to ensure that you develop an effective skin-care routine that ensures the stoma area is thoroughly and consistently cleaned. It's also important to check that you are wearing the correct size ostomy bag to ensure a secure fit, and minimise the risk of leakage. Things like ostomy seals and adhesives can also be useful in cleaning the stoma, and creating a protective barrier to minimise contact with bacteria and other harmful micro-organisms.
Key Features of the Skin Barrier Wipes ✔ Silicone-based skin wipes offer breathable protection Ostomy Bag LeakageOstomy bag leakage is possible the easiest issue to spot on this list. When your ostomy bag is leaking, you will be able to visibly identify the leak as well as see the contents of the bag leaking out. Causes(s) of Ostomy Bag LeakageThere are a wide range of reasons why your stoma bag could be leaking. This includes:
Preventing Stoma Bag LeaksEnsuring that your ostomy bag is the right size and is changed regularly is the best way to help prevent leaking. It's also important to make sure that any supplies you're using are in-date, and clean. You can use an stoma support belt, or wear ostomy underwear, to help protect and support the ostomy bag. Another way to help to prevent leakage is to use an ostomy seal to add an additional protective layer over the ostomy bag.
Key Features of the Trio Genii Ostomy Seals ✔ Also available in a larger, 30 - 50mm ostomy bag size Stoma Bag BlockageThere are two types of stoma blockages; a partial block and a complete block. In a partial stoma block, you may still release a small amount of liquid. In a full stoma block, nothing will come out of your stoma. Stoma Blockage SymptomsThe most severe symptoms of stoma blockage will be easily identifiable (e.g., vomiting and not passing stool). There are a whole range of symptoms, however, which may help you to recognise a stoma block:
Cause(s) of Stoma BlockageThe most common cause of a stoma blockage is a build-up of food, but there are various reasons why a build-up and stoma blockage might occur. This includes improper food digestion, poor stoma hygiene, a twisted or strangled bowel, or local inflammation. Stoma Blockage Treatment The best and most effective way to deal with a blocked stoma is to go to the hospital for medical care. While drinking water, applying heat, or massaging the area may temporarily ease pain and discomfort, a stoma blockage can be dangerous if not dealt with properly.
Key Features of the Physiopack Hot and Cold Pack: ✔ Easy-to-heat by popping the pack in the microwave Stoma Bag BallooningStoma bag ballooning refers to the ostomy bag blowing up due to trapped wind. This is most common with a colostomy, but can also occur if you have an ileostomy. It is important to manage and reduce stoma bag bloating, as severe or long-term bloating can lead to leaking, or cause the entire stoma bag to fall away from your stoma. Cause(s) of Stoma Bag BallooningThere are a few different factors which can contribute to the stoma bag ballooning. This includes:
Preventing and Managing Stoma Ballooning
Stoma Bag PancakingStoma bag pancaking is when the inside of the bag sticks together. This prevents the contents of the bag from filling at the bottom, and can potentially block the bag's filter. Pancaking can also cause your stoma bag to fall from your body. Cause(s) of Stoma Bag PancakingOne factor that can cause stoma bag pancaking is your fluid and fibre intake. If you are not getting enough fluid or fibre in your diet, this can cause stoma bag pancaking. Preventing and Managing Stoma PancakingYou can help to prevent stoma bag pancaking by blowing air into the stoma bag before putting it on. Another option is to roll up a small piece of toilet paper into a small, compact shape (such as a cylindrical, pen-like shape), and drop it into the bottom of the bag. You can also use a drop of oil (such as baby oil) in the pouch to prevent the insides from sticking together. Other Stoma ProblemsOther stoma conditions that it's important to keep an eye out for include: Stoma RetractionStoma retraction refers to a condition whereby the stoma sinks into the abdomen rather than lying on the abdominal wall. While it is less common than other conditions included on this list, it is still worth keeping an eye out for. If your stoma has retracted, you should consult your stoma care nurse about what the best solution for you is. Prolapsed StomaProlapsed stomas occur when a stoma protrudes from the abdominal wall. In this case, the stoma will be swollen and longer than usual. Similar to the stoma retraction, this condition is less common but still worth knowing about if you have a stoma. If your stoma has prolapsed, you should consult your stoma care nurse about what the best solution for you is. Stomal GranulomasStomal granulomas are small red lumps that form on or around your stoma. Sometimes these lumps are not clear or visible, so other symptoms to look out for include bleeding and inflammation in the stoma area. There are a range of causes that could be associated with the development of granulomas, including irritation from leaking faecal matter, friction on the stoma (e.g., when wearing tight clothes), and repeated trauma to the area. The best way to prevent stomal granulomas is to ensure proper care and careful changing of your ostomy bag, using a barrier-cream or barrier wipe when changing your bag, wearing clothing that fits around rather than presses against your stoma (such as ostomy underwear), and ensuring that you are wearing the right size ostomy bag. If you experience symptoms of stomal granulomas, it is important to consult your stoma care nurse for a solution.
Stoma StenosisStoma stenosis, also known as stricture, refers to the narrowing of the opening of the stoma. This can make it difficult to pass urine or stool, and cause the output of the colostomy and ileostomy stomas to become thin or watery. Stenosis is a serious but relatively rare phenomenon. Symptoms of stoma stenosis include nausea and vomiting, trouble with swallowing, and trouble with passing urine or stools. Stoma NecrosisStoma necrosis is a post-operative complication that occurs due to insufficient blood supply to the area. This is an extremely rare condition, and one that you will not be able to treat at home should it occur. Please seek medical assistance if you believe you have stoma necrosis. Symptoms of stoma necrosis include pain and discomfort in the area. You may also notice the stoma change into a darker red or purple colour, or even turn black. Rectal DischargeRectal discharge can occur if you have had a colostomy or ileostomy, but your anus is still intact. In this case, mucus discharge may occur in the anal area due to the lining of the bowels producing mucus that it no longer needs. Rectal discharge can be uncomfortable, but is usually not dangerous. If you find blood or pus in the discharge however, it could be due to an infection, or tissue damage. In this case, it is important to contact your doctor. Understanding the proper stoma care procedures is the best way to prevent a wide range of common conditions that occur with stomas. For more information about life with stomas, and the best way to manage and care for your ostomy bag, we've also written A Guide to Living With a Stoma for new ostomates. Have a question or comment about any common stoma problems? Leave a comment below, or head over to our contact page and drop us a message. |